Anyone who runs a small hospital knows the drill: viral infection season stretches beds, budgets, and staff schedules thin. CorVent Medical enters that picture with a focus on rural health transformation and the simple idea that life-saving care should be more accessible.
Their program ties equipment, remote oversight, and training into one plan so teams can treat complex cases close to home. The result could be fewer transfers, steadier coverage for nights and weekends, and less time spent on logistics when minutes matter.
Why Rural Hospitals Need New Tools
Distance changes everything for critical care. When roads, weather, and transport time stand between a patient and a tertiary care center, every minute matters. CMS’s Rural Health Transformation Program frames the challenge plainly: build local systems that can handle surges, staff constraints, and chronic gaps without breaking.
CorVent aims at that target by packaging ventilatory support with data, workflows, and help built for small teams. That way, rural facilities can make timely choices without sending patients miles away.
What CorVent Brings to the Bedside
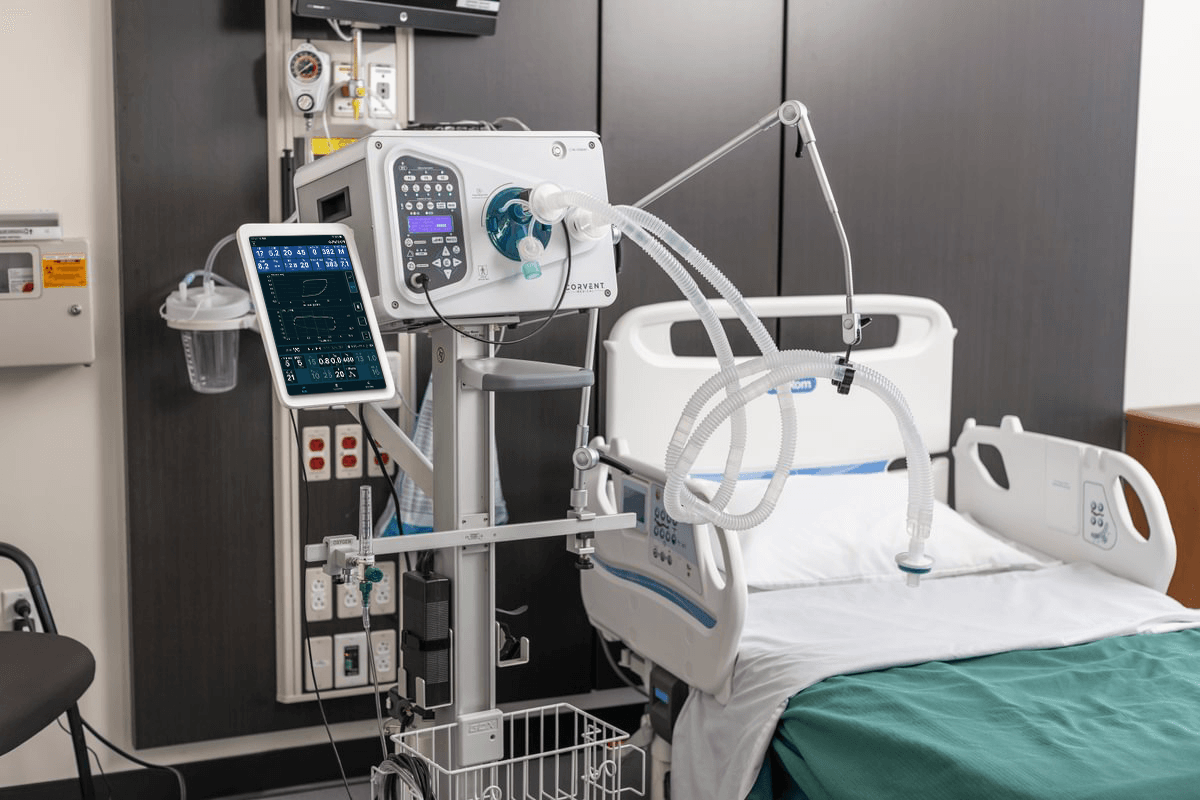
CorVent’s RESPOND ventilators emphasize reliability and ease, featuring modes that cover common respiratory needs and interfaces that are designed for mixed-experience teams. Paired with the CorVision gateway, clinicians can view trends and changes for multiple patients at once, with the information displayed on a central screen and integrated into their facility’s electronic record platform.
The practice said, “Through our RESPOND ventilators and CorVision remote monitoring platform, we enable rural hospitals and critical access facilities to manage complex patient care locally, reducing the need for transfers to urban centers and improving patient outcomes.” CorVent Medical positions itself as a practical bridge between bedside care and remote expertise.
Preparedness, Without Overbuilding Capacity
Rural facilities plan for slow weeks and sudden surges. CorVent’s approach treats preparedness as a flexible layer: devices on site, with remote monitoring available, and protocols ready to activate when a respiratory event hits.
That mix may help hospitals respond to storms, flu season, smoke seasons, or community outbreaks without scrambling for borrowed equipment or last-minute staff. It could also keep care local when helicopters are grounded, and transport is impossible or too costly to deploy. The goal is simple enough: have the right tools at hand, then scale effort only when needed.
Data That Lightens the Workload
Small teams are prepared to take on multiple roles. CorVision pulls ventilator data into one view, highlights changes worth a second look, and shares status with care partners in real time. The aim is to reduce repeated trips from room to room, help small teams spot issues early, and support clinicians with information instead of guesswork.
For the clinician, this could mean more efficient rounds, faster handoffs, and fewer back-and-forth calls. Training and usability also matter, so CorVent pairs deployments with support that keeps new users confident at the bedside.
Local Care, Bigger Long-Term Gains
Moving fewer patients can protect families from travel costs and time away from work, and caring for patients in their communities empowers rural healthcare systems and providers, enabling their long-term survival. It may also free up regional ICUs for cases that truly require transfer, ensuring all patients receive the level of care they need.
CorVent is looking to expand this model, aligning its plan with CMS’s push for sustainable, locally managed critical care. Over time, the combination of RESPOND devices, CorVision oversight, and staff coaching could help rural hospitals keep more care close to home.
This article is for informational purposes only and does not substitute for professional medical advice. If you are seeking medical advice, diagnosis or treatment, please consult a medical professional or healthcare provider.